Where does the future of medicine lie? Perhaps in our intestines.
By Aditya Uppuluri
Recent research suggests that the secret to tackling conditions such as atherosclerosis (accumulation of plaque in arteries), cancer, and even autism may involve the small and large intestines. But how? How it is that two parts of the body, that are technically located outside of the body (yes, the inside of the digestive tract is technically outside of the body), may be the keys to addressing some of the most difficult-to-treat health conditions? The answer is the Gut Microbiome.
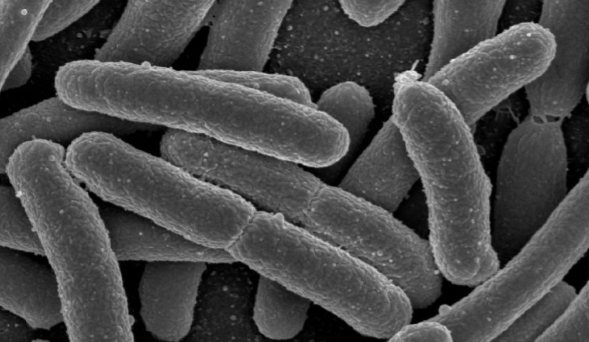
The Gut Microbiome refers to all of the bacteria that inhabit the human gut. The small and large intestines are home to a large amount of non-pathogenic bacteria. While the exact population of bacteria is not known, estimates suggest that bacterial cells outnumber body cells by a ratio of 10 to 1. The reason this possible is that bacterial cells are much smaller than human body cells. In most cases, the Gut Microbiome and human body cells coexist without conflict; the Gut Microbiome actually serves some important protective and metabolic functions. Because of the numerous functions that it performs, many scientists consider the Gut Microbiome to be one of the most important endocrine organs in the body. Being an “endocrine organ,” the Gut Microbiome is able to cause a variety of effects on the body; recent research posits that the Gut Microbiome may affect the risk of developing cardiovascular disease, the onset of autism, and the effectiveness of cancer treatments.
The effect of the Gut Microbiome on the development of cardiovascular is a relatively recent research topic that has the potential to revolutionize the way that scientists address cardiovascular disease. To understand the impact of the Gut Microbiome on cardiovascular disease, it is important to remember that the primary source of nutrition for the Gut Microbiome is the food we eat; the bacteria in our gut get the “leftovers” that we do not digest and absorb. Now here’s the interesting point: certain types of bacteria in our gut are able to take up the food we eat and convert it into a substance whose presence in the blood in significantly correlated with an increased risk of developing cardiovascular disease. The substance is called trimethylamine N-oxide (TMAO), and high levels of TMAO in the blood have been associated with a greater build up of atherosclerotic plaque. Of the food we eat, red meat (steak, hamburgers, ribs, etc.) is especially dangerous because the bacteria metabolize parts of it, leading to an increased risk of developing cardiovascular disease. The point: bacteria in our gut are able to secrete substances, based on the food we eat, that can increase our risk of developing cardiovascular disease.
While there is a well-researched link between the Gut Microbiome and cardiovascular disease, new research is starting to emerge regarding the Gut Microbiome and a potential link to autism. Autism is a condition that is associated with the brain and cognitive development. However, studies have shown that as many nine out of ten people with autism suffer from a gastrointestinal problem. Additionally, analysis of fecal matter showed that there was a significant difference in the microbial-products between autistic and non-autistic children.
Further studies sought to determine whether this was a cause or effect of autism. One of the studies involves creating an autism-like syndrome in the offspring generation of mice by injecting pregnant mother mice with a virus-like molecule. When the offspring were born, the ones with the autism-like syndrome had a significantly different Gut Microbiome than healthy mice. The mice with the autism-like syndrome were then exposed to Bacteroides fragilis, which is a health-promoting bacterium. The result was that exposure to the “good” bacteria led to an improvement in the behavior of mice with the autism-like syndrome; the mice were less anxious and they had better vocal interactions with other mice. The possibility: altering the Gut Microbiome through probiotics (healthy bacteria) may impact autism. The mechanism by which the Gut Microbiome affects autism is an area of ongoing investigation. Because autism syndrome involves a complex interplay of genetic and environmental factors, more research needs to be done to determine whether or not the Gut Microbiome will be an effective target for managing autism.
In addition to autism and atherosclerosis, the Gut Microbe also significantly affects the effectiveness of anti-cancer immunotherapy. There are many ways of addressing cancer, and one means of doing so is to use a class of medications called “checkpoint inhibitors.” The role of these inhibitors is to allow immune cells to effectively attack and destroy cancerous cells. As it turns out, the effectiveness of the drug varies from person to person. In some percentage of the population, a “checkpoint inhibitor” works successfully, but in another percent of the population, the effects are subpar. To account for this discrepancy, scientists point to the Gut Microbiome. Studies have demonstrated that the effectiveness of some “checkpoint inhibitors” hinges on the patient having the right combination of gut bacteria. Mice studies have revealed that mice without Bacteroides thetaiotamicron and Bacteroides fragilis did not show as good results when treated with “checkpoint inhibitors” as mice that did have the two bacteria. Furthermore, when mice were exposed to the two healthy bacteria, the effectiveness of the medications significantly increased. While the mechanism by which the Gut Microbiome effects this change is not fully known, it will be a target of further research. The point: to be fully effective, anti-cancer immunotherapy requires the presence of a proper and healthy Gut Microbiome.
The Gut Microbiome is one of the unexplored frontiers of medicine; it is evident that the Gut Microbiome may revolutionize the way physicians tackle certain health conditions. While it is good to be optimistic, it is important to be practical; at the moment, more research needs to be done to verify the mechanisms by which the Gut Microbiome contributes to these health conditions. Once the mechanism is verified, scientists can begin developing drugs that alter the mechanism to effectuate a certain change in the body. Because of the vast potential of the Gut Microbiome, we can conclude that it will play a significant role in the Future of Medicine.